USA DENTAL SOLUTIONS
USA Dental Solutions is a progressive, customer oriented dental practice management & IT services company based out of Houston, Texas.
We are a leading national Revenue Cycle & Business Management Consulting provider catering to dental practitioners in the United States.
Revenue Cycle Management
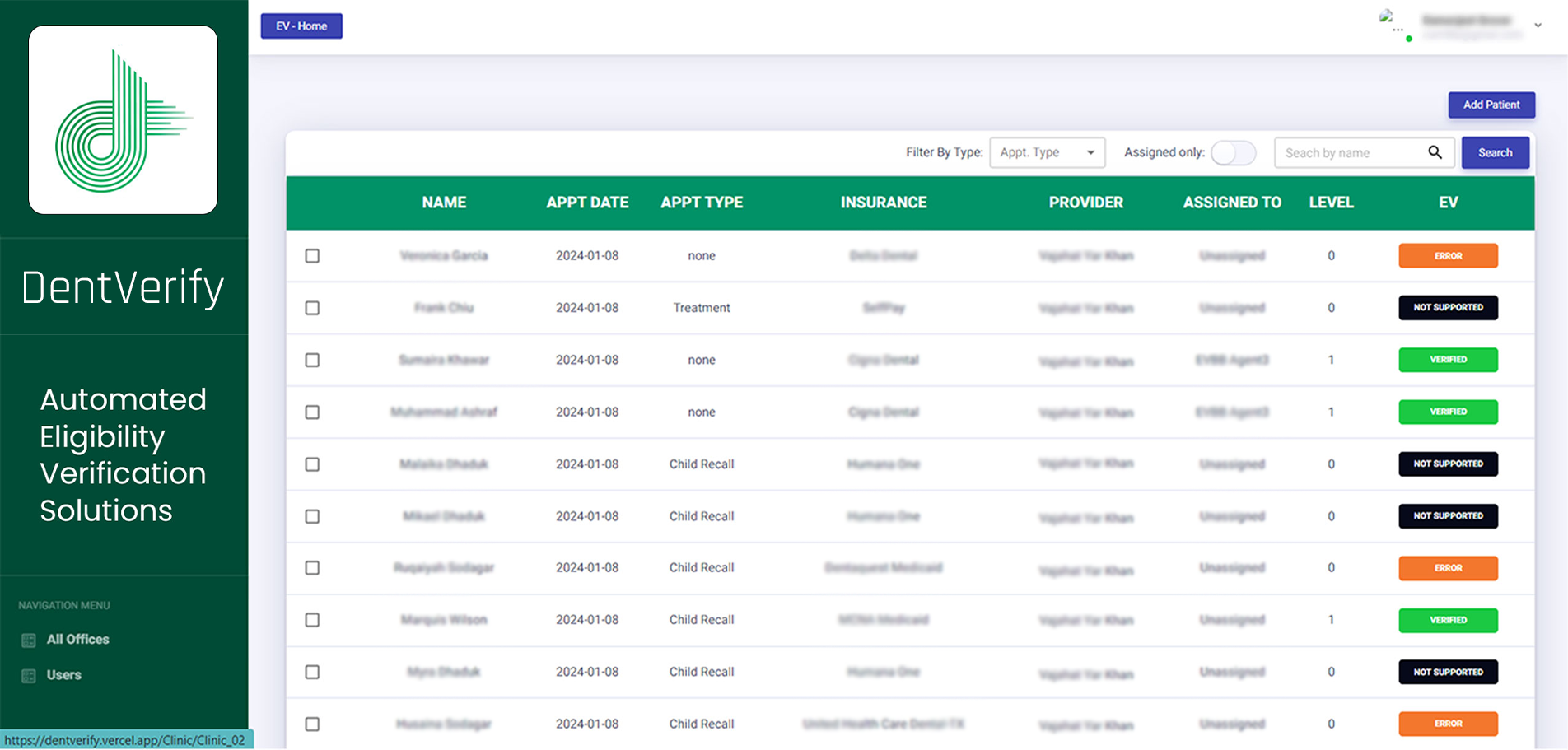
Insurance Verification
Patient insurance eligibility verification is the starting point of the RCM process and undeniably the most important. Claim denials due to errors in the verification process occupy the top spot in the list for rejections of payor payments.
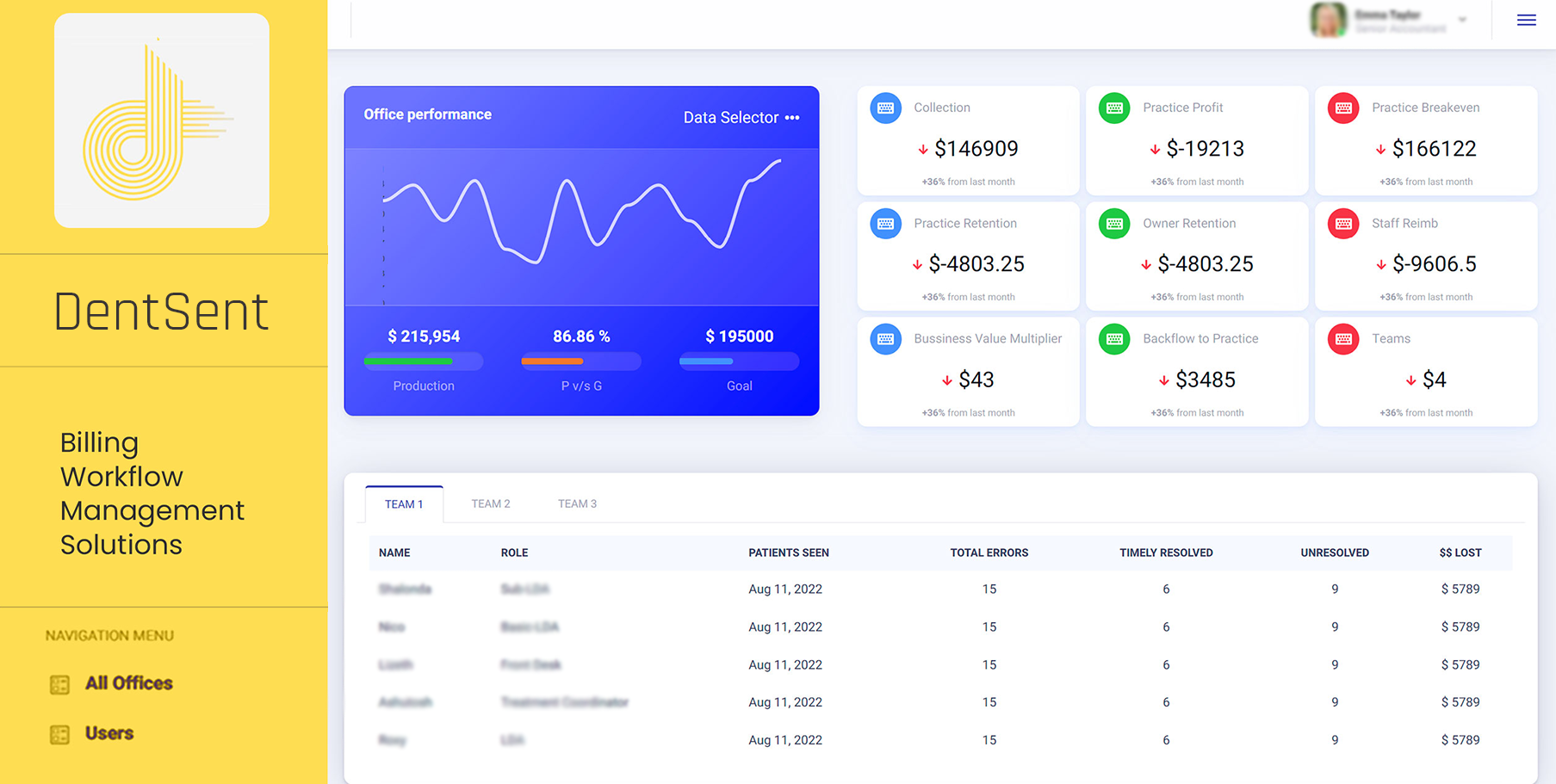
Billing
Our specialists review the charts, notes and dental claim for accuracy. This process ensures that claims are clean and will significantly increase first-pass payments and reduce claim denials.
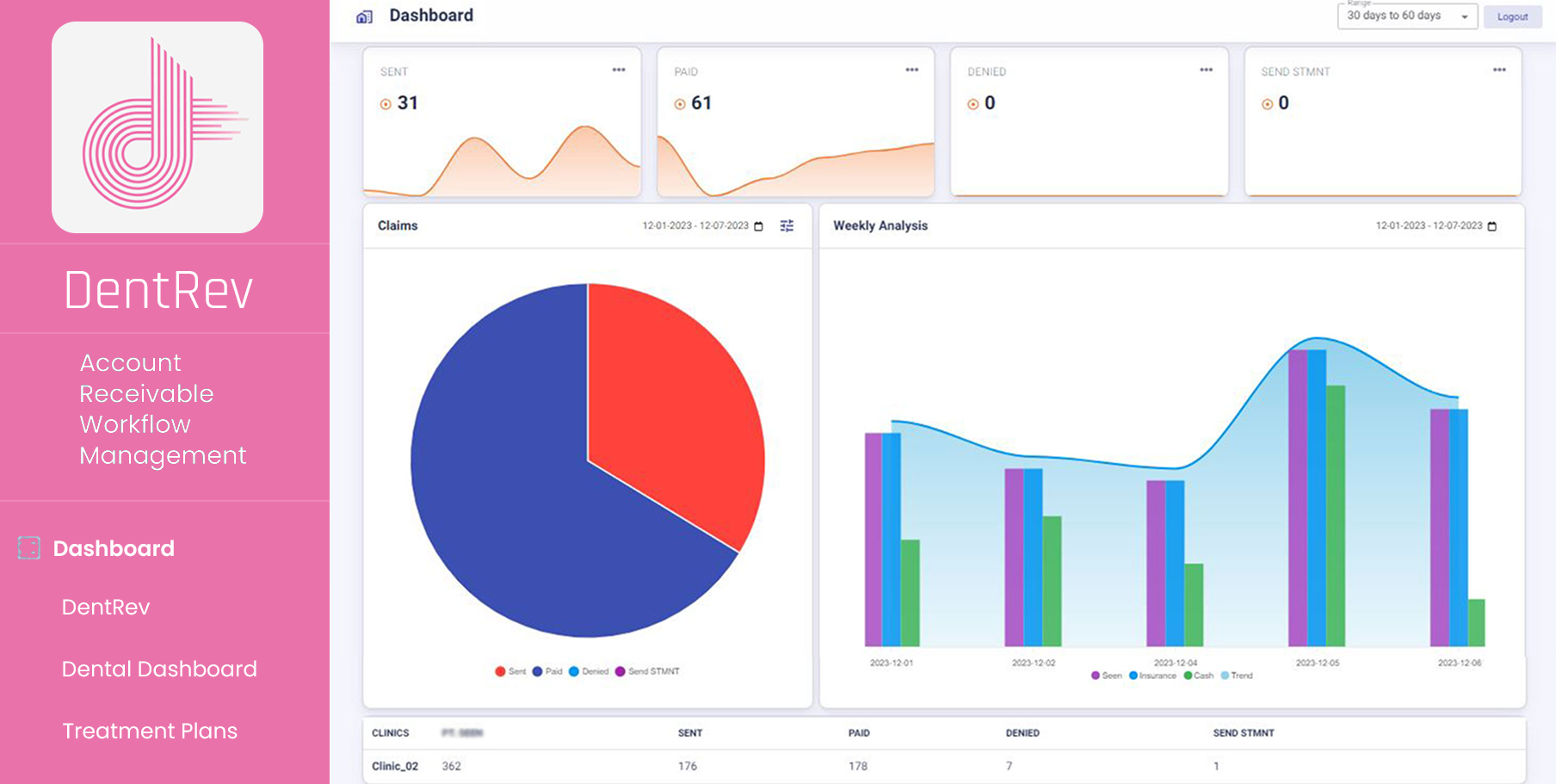
Account Receivables
The service is designed to ensure that our clients collect every cent that possibly can be collected from the AR which is sitting in the < 60 & <90 days bucket. Our calling and denials resolution teams work dedicatedly towards fighting for the hard earned money of our clients.
What Makes us Better
As a responsible revenue cycle management company, we understand that process optimization is critical for the growth of a healthcare company, consequently we take utmost care to constantly upgrade our services to the next level.
Effective Communication – Patients who are well-informed understand their financial obligations quicker, and are more likely to have a positive healthcare experience.
Leveraging Human Capital – By leveraging human capital we maximize their potential which increases production and thus profitability.
Adherence to guidelines – We are firm on regulatory compliance as it ensures integrity and promotes the overall quality of care while safeguarding patients’ rights.
Improved Collections
Reduced Costs
Our clients have reported up to 30% reduction in their operational expenses post signing up with us.
Customer Success

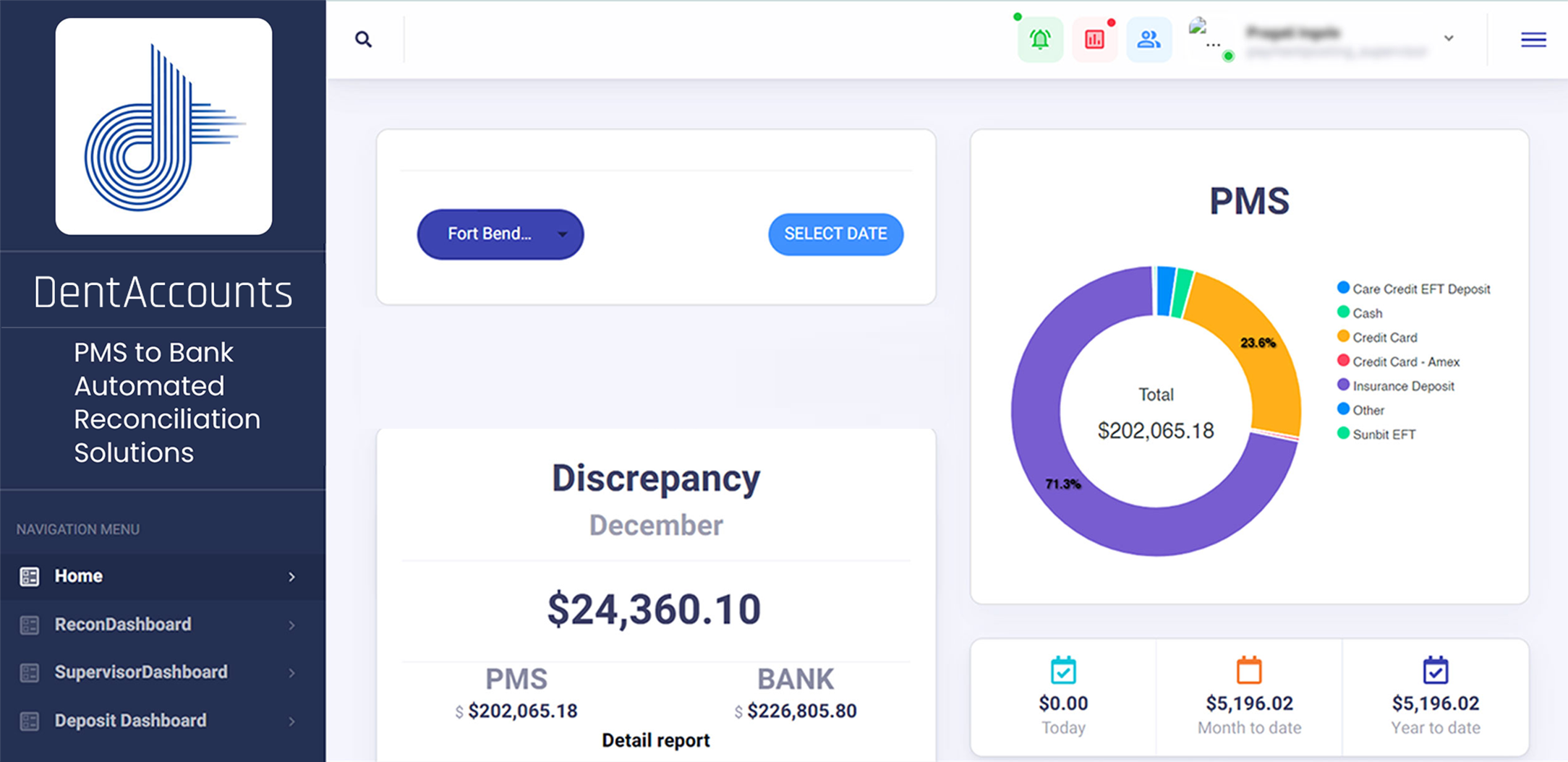
DentTracks is All in one Dental Patient Management Software (PMS) Aggregator Centralized, Cloud-Based Solution
DentTracks offers a cloud-based Dental IT solution custom configured, standardized and optimized to the practice and its workflows. Cloud-based Software-as-a-Service (SaaS) system, with reduced up-front cost including FREE maintenance, support and upgrades. Our servers are hosted with industry leading cloud services that guarantee 99.9% uptime with reduced liability compared to onsite systems. DentTracks maintains data security in accordance with HIPAA and PCI compliance. Minimum computing skills and experience required to use DentTracks.
Why Choose us?
We understand the difficulties faced by officers and managers with regards to the workload and constant challenges being faced when it comes to managing patients, employees and the practice financials.
Our aim and goal are to be a one-stop solution for all our clients. The best part of our offerings is the ease of selecting the desired services without any restrictions and on an as-needed basis.
NO LONG TERM CONTRACTS
NO DISRUPTION IN DAILY ACTIVITIES
SELECT THE SERVICES YOU NEED
OFFICER MANAGER’S BEST FRIEND
INCREASED CASH FLOWS
DECREASED OVERHEADS
Kind words from online
industry leaders


Frequently Asked
Questions
We provide end-to-end RCM solutions including patient billing, coding, claims processing and denial management.
RCM improves cash flow, reduces billing errors, and increases a healthcare organization’s overall financial efficiency.
Our RCM platform has powerful compliance capabilities to comply with industry standards and regulations to ensure data security and integrity.
Our RCM system ensures compliance with healthcare regulations by using advanced algorithms and regular updates. This minimizes the risk of regulatory penalties.
Our platform optimizes reimbursement rates for healthcare providers through data analytics and predictive modeling.
We prioritize seamless interoperability and integration with diverse healthcare IT systems.
We safeguard patient data and ensure HIPAA compliance through stringent data security protocols.
Our RCM system can adapt to changes in billing codes and industry standards.
We address denials and rejections in the revenue cycle by using denial management algorithms and proactive analysis. This leads to a more streamlined revenue cycle.